Surgical instrument management in european hospitals: 4 blind spots


This article explores common yet overlooked blind spots in surgical instrument management within European hospitals. It is grounded in direct field research conducted in collaboration with hospital staff, and enriched by academic insights from our cofounder, Kaat Dhondt, PhD researcher at the University of Antwerp. By combining real-world observations with academic perspectives, we aim to highlight critical inefficiencies hospitals often encounter - inefficiencies that remain hidden yet significantly impact costs, sustainability, and operational effectiveness.
Hospitals today face increasing pressures from multiple angles: rising patient numbers, tighter schedules, stricter regulatory requirements, and ambitious sustainability goals. Within this demanding landscape, managing surgical instruments — critical, costly, and reusable resources — becomes particularly challenging. Staff shortages and time constraints further complicate the task, leaving OR nurses, sterilization staff, and logistics teams frequently operating under stressful, suboptimal conditions.
The complexity of the surgical instrument workflow magnifies these pressures. Sets move constantly between operating rooms, sterilization departments, and storage areas. Instruments pass through multiple hands, are used in rapid succession, and must meet rigorous standards for cleanliness, completeness, and traceability. As demands rise, even small disruptions or losses in the system can quickly compound into substantial operational, financial, and environmental costs.
This context creates precisely the kind of blind spots that undermine efficiency, reliability, and sustainability in hospitals. In the sections that follow, we outline four key blind spots identified through our research, explain why they persist, and discuss how hospitals might close these gaps.
The operating room is the most fast-moving, high-risk, and tightly scheduled environment in a hospital. Yet, it’s also one of the least supported when it comes to managing surgical instrument sets - especially in the crucial moments after surgery ends. This short window represents the last realistic opportunity to detect missing or misplaced instruments before they leave the OR or nearby utility rooms to be processed by the Central Sterilization Department (CSD).
A significant reason why this moment is so challenging lies in the inherent complexity and fragmentation of the OR workflow itself. The handling of surgical instrument sets involves multiple quick handovers, decisions made under pressure, and actions performed across different zones - often without standardized protocols or consistent tracking.
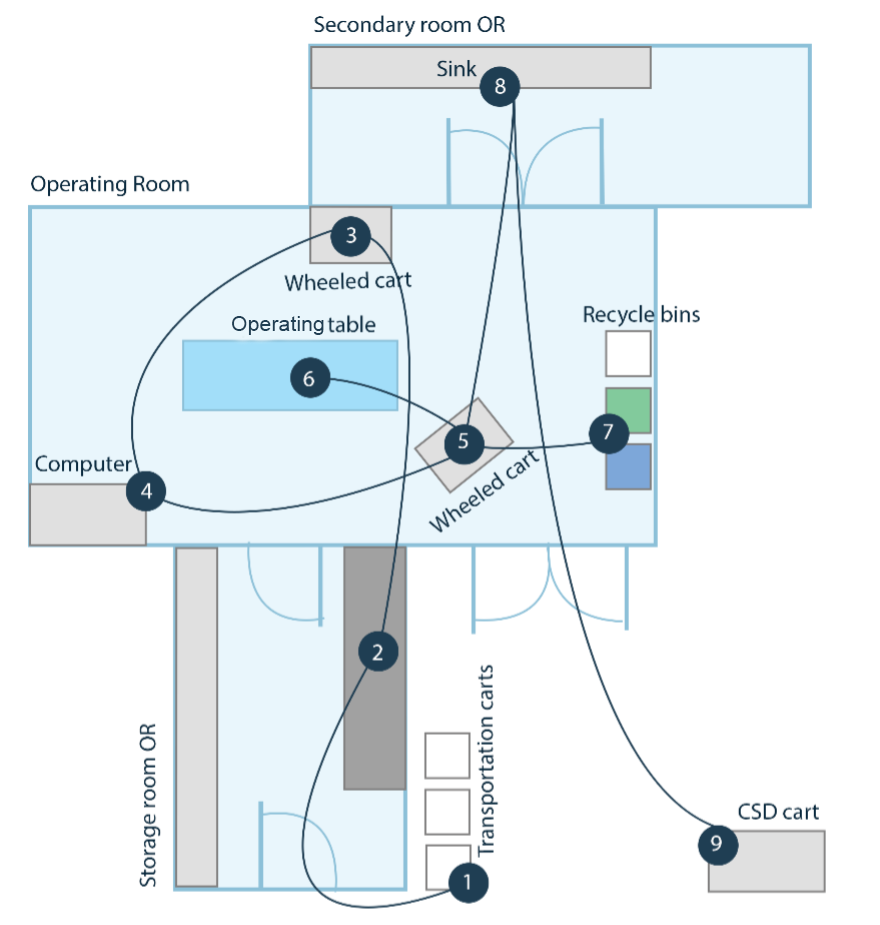
A simplified overview, based on field research conducted at a Belgian university hospital, illustrates the number of small but critical actions required to handle sets before, during, and after surgery. Each step - opening sets, distributing instruments, clearing tables, and checking baskets - is time-sensitive and vulnerable to errors, increasing the likelihood of instruments being misplaced, swapped between baskets, or going unreported.
If only one set is involved, detecting and recovering a missing instrument may be straightforward. But when multiple sets have been used, tracing a single missing instrument becomes complicated and time-consuming, sometimes taking staff up to 20 minutes of manual searching. Without clear tracking systems or structured guidance, staff are left guessing: Was it discarded accidentally? Is it in another basket? Or was it simply overlooked?
Existing solutions to check set completeness rely heavily on structured and controlled environments – like the CSD -, assuming neatly organized sets. Yet this assumption rarely holds true after a busy surgical procedure, where instruments have been thrown back in the baskets without putting a lot of effort in making sure it’s done tidy.
What's missing is direct support to quickly clarify what's missing, and that offers immediate guidance to resolve discrepancies without adding extra burden to an already overloaded team.
When a missing instrument is identified — usually through quick manual counting or a basic weighing system — the instinct in hospitals is straightforward: replace the instrument immediately with a sterile spare and move forward. On the surface, this action achieves its immediate goal: procedures continue without delay, and patient care isn’t compromised. But beneath this quick solution lies a deeper issue that remains unaddressed and untracked.
Current detection methods like weighing scales or manual counts alert staff to the presence of a problem, but provide no intuitive guidance for resolving it. Hospital teams, already under intense time pressure, frequently spend significant effort manually searching through multiple baskets or sets, trying to locate the missing item. Without structured instructions or clear responsibilities, these searches become inefficient, frustrating, and often inconclusive.
Moreover, responsibilities are often fragmented across teams: OR staff quickly fix the problem to stay on schedule, rarely logging the loss; sterilization staff assume incoming sets have already been validated, missing opportunities to track down what’s lost; logistics sees stock depletion without context, unable to trace it back to specific incidents. Because of this disjointed approach, instruments quietly disappear from stock, and these small incidents compound into larger, systemic issues.
In essence, immediate actions surpass their intended goals: solving short-term disruptions at the expense of understanding long-term trends. Without an integrated system linking each detected issue to a clear recovery action and outcome, hospitals remain stuck addressing symptoms instead of resolving root causes.
Hospitals depend heavily on maintaining accurate and predictable stock levels of surgical instruments. Yet the reality is that most hospitals struggle with stock transparency at two critical levels, both directly influenced by the challenges discussed earlier.
On one level, missing instruments are often resolved with immediate, undocumented replacements. While this approach ensures surgeries continue without interruption, it leaves the hospital unaware of how often and where instruments are actually lost. Without systematically logging these incidents, hospitals lack the data needed to identify patterns and hotspots-specific procedures, departments, or circumstances where instruments routinely go missing. As a result, they miss crucial opportunities to proactively prevent loss, tackle root causes, and optimize their workflows.
At another level, not all missing instruments are truly lost in waste bins or accidentally left in patients. Often, they’re simply misplaced — ending up in the wrong basket or set. If this misplacement isn't caught immediately after surgery, the CSD staff notice a missing instrument and understandably place a spare instrument into the set. Eventually, the misplaced instrument reappears in the wrong basket, leading to confusion and inaccuracies. Over time, this repeated misalignment makes stock management increasingly unreliable. Hospitals lose track of how many instruments they truly have available, triggering unnecessary reorders, inflated inventory, and avoidable costs.
Together, these two intertwined transparency gaps leave hospitals struggling to manage their surgical instrument inventories efficiently. Without clear and accurate visibility into their true instrument stocks, hospitals remain stuck in a costly cycle of reactive ordering and chronic uncertainty - replenishing items they might already have, simply because they're hidden elsewhere in the system.
Beyond operational inefficiencies, surgical instrument management carries a hidden sustainability impact that's often overlooked. When an instrument is discovered missing late in the process of preparing for a surgery, hospital staff commonly resort to pulling a spare from stock or opening an entirely new set. While this immediately resolves the issue, it triggers a resource-intensive cascade. Even if just one instrument is needed, the remaining unused instruments must still undergo full reprocessing, consuming substantial amounts of water, energy, and disposable packaging materials.
Since these small losses are rarely documented, the true environmental footprint remains hidden. Hospitals actively track visible sources of waste or energy consumption, yet the cumulative environmental cost of extra sterilization cycles, redundant packaging, and unnecessary instrument replacements often goes unnoticed. Over time, these seemingly minor inefficiencies compound into significant but unrecognized environmental harm. Addressing this sustainability blind spot means improving visibility and early detection of missing instruments, allowing hospitals to avoid unnecessary reprocessing, extend the useful life of instruments, and meaningfully reduce their environmental impact.
Lynqo addresses the blind spots in instrument management by providing hospitals with clear visibility at precisely the moments and places it’s needed most. Our solution detects missing and misplaced instruments directly after surgery, ensuring teams can quickly and intuitively resolve issues before they escalate into hidden losses, operational delays, or sustainability impacts.
By linking detection directly to structured and actionable follow-up steps, Lynqo ensures transparency across departments, clarifies responsibilities, and helps hospitals prevent chronic instrument loss at its source. The result: fewer disruptions, less waste, improved instrument availability, and a more sustainable, efficient surgical environment.